Recently, America mourned the death of a woman known as the Queen of Soul, Ms. Aretha Franklin. While her life and all that she gave to the world were celebrated in grand fashion, many of us wondered about the illness that caused her death and whether we or our loved ones could be at risk for it.
Pancreatic cancer. Known for its voracity and ability to cause a painful death, those who are familiar with it understand why it invokes fear.
Many are asking if they might be at risk, and if so, what can be done about it.
The truth of the matter is that pancreatic cancer is a rare diagnosis, one for which the average person will have few, if any, risk factors. That’s the good news.
The not-so-good news is that there is no effective screening test to determine who truly might be at risk. And unfortunately, that is the case for most cancers.
It is important to understand that when you go to your annual preventative exam with your healthcare provider, you are not likely to be screened for every cancer that exists. Screening tests are administered based upon the following criteria:
- The frequency with which a given disease occurs in the general population;
- Risk factors that a patient may have, including age, gender, family history, prior illness and known environmental exposures;
- Whether or not there is an effective SCREENING test for the disease;
- Whether or not your insurer will cover the cost of the test, which is contingent upon the responses to criteria 1-3.
Before going any further, however, it is important that you understand the difference between a screening test and a definitive or diagnostic study. Not only should you understand the difference between the two, but you should also know the criteria for a screening exam to be considered effective.
So, what is a screening test?
A screening test is a clinical exam that, does not determine who has a given disease; but determines who may be at significant risk of having the disease. While it occasionally does accurately predict the presence of the disorder in question, its true utility is that it is a signal that further testing is necessary to determine the presence of absence of disease.
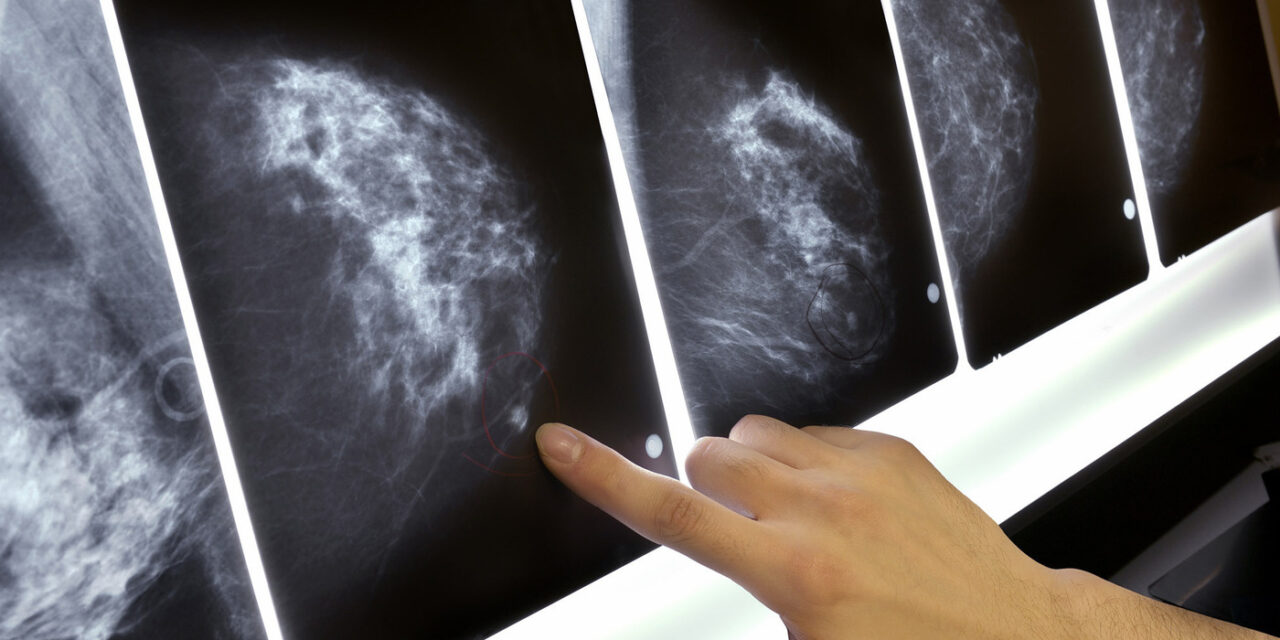
For example, a mammogram is a screening test for breast cancer. While images obtained by the mammogram may be highly suspicious for cancer, they do not establish beyond a shadow of a doubt that cancer is present. They simply indicate that further testing is required. Sometimes the follow-up exam will be an ultrasound; and often it will be a biopsy. The biopsy is the “gold-standard test” and definitive, as it obtains actual tissue for further analysis and will indicate the presence of cancerous or pre-cancerous cells.
What is a definitive or diagnostic test?
A definitive test is that test which proves that a disease is present and indicates the need for treatment. Again, the biopsy is the definitive study which would be used to establish a diagnosis of breast cancer.
What are the criteria by which a screening test is established?
- It must be used in a population in which the disease being studied is prevalent. In other words, we do not screen infants for high cholesterl because we know that they are unlikely to have it.
- It must be a disorder which is known to cause significant suffering or death;
- It should be relatively non-invasive; meaning that the implementation of the test should not pose significant risk to the patient. Risk in this case is defined as the risk of infection, hemorrhage or inadvertent injury as a result of the test. (There are exceptions to this, but as a general rule, it is true.)
- It should be a relatively inexpensive test. Again, there are certain exceptions to this rule, but even in these cases, the cost of the screening test far outweighs the expense that would be incurred if the disease was to be present;
- It is always used to detect cancer before the occurrence of signs and symptoms.
So, what are the malignancies for which you can be screened, assuming that you have none of the risk factors below, but are having a simple preventative visit? And what does screening for the standard cancers typically entail? What are the follow-up exams that you might undergo if any of these routine screens are positive?
(Disclaimer: If it is documented that a patient has any of the risk factors below, or is symptomatic for a specific cancer, then certain tests, which fall outside of the scope of this article, are performed. However, these tests would not be offered standardly to the population at large. The tests below refer only to individuals without any documented risks.)
| CANCER TYPE | RISK FACTORS | IS THERE A STANDARD OR ROUTINE SCREENING TEST? | SCREENING TEST | FOLLOW-UP TEST(S) |
| Ano-Rectal | HPV; HIV; smoking, multiple sex partners; immune compromise; previous cervical, vaginal or vulvar cancer | No | ||
| Bladder | Smoking; workplace exposure to aromatic amines and organic chemicals; use of Actos for > 1 year; Caucasian race; chronic bladder irritation; not drinking enough fluids; family history; Lynch syndrome; RB1 gene mutation; bladder-related birth defects | No | ||
| Bone | Genetic disorders; Paget’s Disease; History of radiation exposure; Metastatic cancer from a different organ | No | ||
| Brain | Radiation exposure; Family history; Multiple genetic conditions; Metastatic cancer from a different organ | No | ||
| Breast | Family history; BRCA; Lynch Familial Syndrome; age > 50; menses prior to 12 yo; Never pregnant; 1st pregnancy after 30 yo; birth control pills; obesity; alcohol consumption; menopause after 55 yo; postmenopausal hormone therapy; use of DES; North American residency; meat consumption | Yes | Mammogram | 1. Biopsy;
2. Possible ultrasound |
| Cervix | HPV; multiple sexual partners; other STDs; weakened immunity; obesity; low income; maternal history of DES exposure; smoking | Yes | Pap Smear | 1. Colposcopy;
2. Possible ECC; 3. Possible biopsy |
| Colon | Family history; North American residency; age > 50; history of colorectal polyps; history of inflammatory bowel disease; obesity; sedentary lifestyle; diet high in red meat; smoking; heavy alcohol consumption; Lynch Familial Syndrome and other genetic syndromes | Yes | At age 50, if no other risk factors:
1. Digital rectal exam; 2. Occult blood study; 3. Colonoscopy |
|
| Esophageal | Gastro-Esophageal Reflux Disease; Barrett’s esophagus; use of tobacco; alcohol consumption; obesity; diet high in nitrogenous substances, like processed meats; achalasia; Plummer-Vinson Syndrome; chemical injury to the esophagus; smoking; history of throat, mouth or lung cancer; HPV | No | ||
| Leukemia | Exposure to high doses of radiation; smoking; exposure to radiation or chemotherapy for prior cancer treatment; myelodysplastic syndromes; genetic syndromes; family history | No | ||
| Liver | Asian American race; Pacific Islanders; Hepatitis B; Hepatitis C; cirrhosis; Fatty liver (non-alcoholic); Primary biliary cirrhosis; obesity; heavy alcohol consumption; use of anabolic steroids; smoking; Hereditary hemochromatosis; other rare metabolic and genetic disorders | No | ||
| Lung | Smoking; family history; Asbestos exposure; Radon exposure; cancer-causing chemicals in the workplace; pollution | No | ||
| Lymphoma | History of mononucleosis; weakened immunity; family history; exposure to benzene and certain pesticides and herbicides; history of chemotherapy or radiation; HIV; Hepatitis C; H. pylori | No | ||
| Multiple Myeloma | Age > 65; African American race; family history; obesity | No | ||
| Ovarian | Family history of ovarian, breast or colon cancer; First pregnancy after 35 yo; no history of full-term pregnancy; history of IVF; hormone replacement therapy after menopause; BRCA mutation(s); Lynch Familial Syndrome; history of breast cancer | No | ||
| Pancreatic | Smoking; obesity; workplace exposure to chemicals; age > 65 yo; African American race; family history; genetic family syndromes; diabetes; chronic pancreatitis; cirrhosis | No | ||
| Penile | HPV; HIV; not circumcised; smoking; phimosis; smegma | No | ||
| Prostate | Family history; age > 50; African American race; Afro-Caribbean ethnicity; North America, Northwest Europe, Australia and Caribbean residents; BRCA gene mutations; Lynch Familial Syndrome | Yes | 1. (Digital rectal) Prostate exam;
2. Prostate Specific Antigen (PSA) |
1. Prostate ultrasound;
2. Possible biopsy |
| Skin | Lighter skin; family history; history of sun burns and extensive tanning; blue or green eyes; blond or red hair; certain types of moles | No | ||
| Stomach | Age > 50; Asia and South and Central America residency; H. Pylori; diet heavy in smoked, salted and pickled foods; smoking; obesity; prior gastric surgery; pernicious anemia; stomach polyps; family history; multiple genetic family syndromes; history of mononucleosis; work in coal, metal or rubber industry; weakened immunity | No | ||
| Testicular | Undescended testicle; family history; HIV; ages 20-34; Caucasian race | No | ||
| Uterine | Menses before 12 yo; never pregnant; Tamoxifen use; family history; obesity; diet high in fat; polycystic ovarian syndrome; ovarian tumors; history of breast or ovarian cancer; endometrial hyperplasia; Lynch Familial Syndrome | No |
This guide is by no means meant to be exhaustive. There are many other elements that it has not mentioned, that can arguably be viewed as risk factors, even though they do not fall among the commonly known issues. Please use this as a starting point for discussion between you and your provider as to the best course of action for you to pursue. Remember that each year, your risk profile for each of these may change as you age, as your exposures vary, as your family medical history evolves and as you develop other medical concerns and conditions. In other words, your risk for certain diseases may increase OR decrease over time. Keep the dialogue between you and your physician fresh… and always remember to be your own best advocate!